
Suboxone is a prescription medication used to treat opioid use disorder. It combines buprenorphine, which partially activates opioid receptors to reduce cravings and withdrawal, and naloxone, which helps prevent misuse.
Growing up with a parent who struggled with drug and alcohol use, I saw firsthand just how unclear and complicated the path to recovery could often be. Thankfully, medications like Suboxone have made it easier for many people to reduce their opioid use and start feeling more in control of their lives.
While highly effective, there's still some confusion around how Suboxone works, and misunderstandings about opioid medicines can have real consequences. Even though Suboxone and other drugs work well, research shows that only 25% of people in the U.S. get medication to treat opioid use. This is why the availability of high-quality information, and accessible resources is so essential.
Getting treatment can be hard for many reasons. Appointments can be tough to schedule, clinics may be far away, insurance can be confusing, and some medications have extra rules that make them harder to get. Boulder helps fix this by making proven treatments more accessible while removing unnecessary obstacles.
If you have questions about Suboxone, this article will make things clearer. We'll walk through how this medication works and why it's used to treat opioid use disorder. We'll also talk about what treatment can realistically look like, including the ups, downs, and flexibility that's built into long-term care.
Suboxone is a prescription medication used to treat opioid use disorder. It is usually taken once a day as a dissolvable film or tablet placed under the tongue or inside the cheek. Its generic name, buprenorphine/naloxone, refers to the two medicines it contains, each of which serves a specific purpose:
Buprenorphine is available in several formulations, including the dissolvable Suboxone and Zubsolv, as well as the long-acting injections Sublocade and Brixadi. Most formulations combine buprenorphine with naloxone, which is included to discourage misuse by injection.
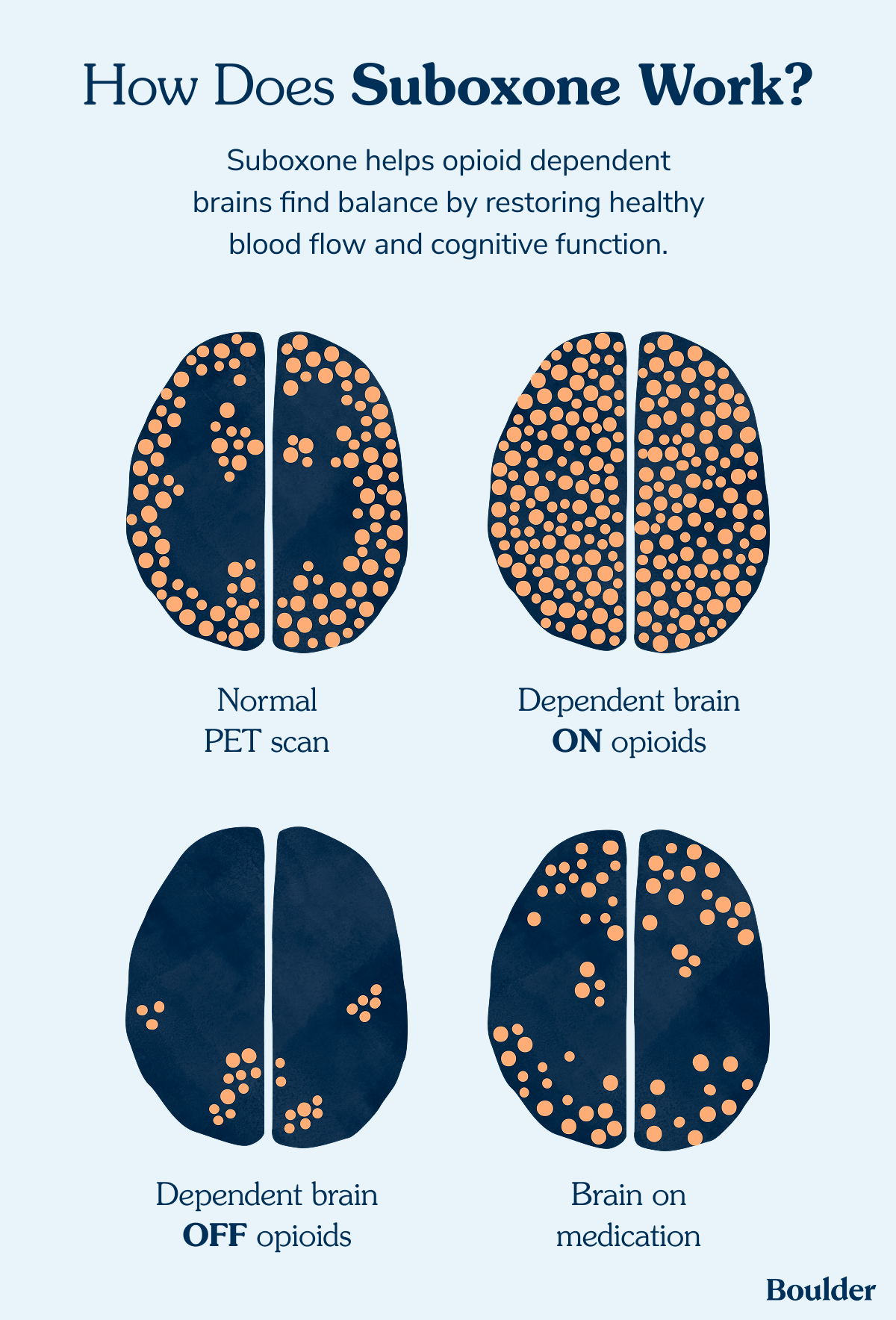
Opioids affect receptors throughout the brain and body, particularly those involved with mood, pain, and breathing. Most opioids become more dangerous when taken in larger amounts, which is why overdose can happen.
Buprenorphine works differently. It binds tightly to the opioid receptors but doesn’t activate them all the way. That helps ease withdrawal and cravings without the intense rush or sedation caused by other opioids.
Suboxone is a medicine that helps people who are recovering from opioids. It stops the painful parts of quitting, reduces your risk of overdose, and calms your cravings. “Buprenorphine creates stability so people can get back to their lives. When someone isn’t constantly battling withdrawal or cravings, they can focus on what matters–their families, their work, their goals,” says addiction medicine physician Dr. Ayesha Appa.
Boulder's treatment focuses on making someone's situation safer and more stable right now. The aim is to lower risk, improve quality of life, and make it easier to move toward recovery goals. That happens best when it fits into real life.
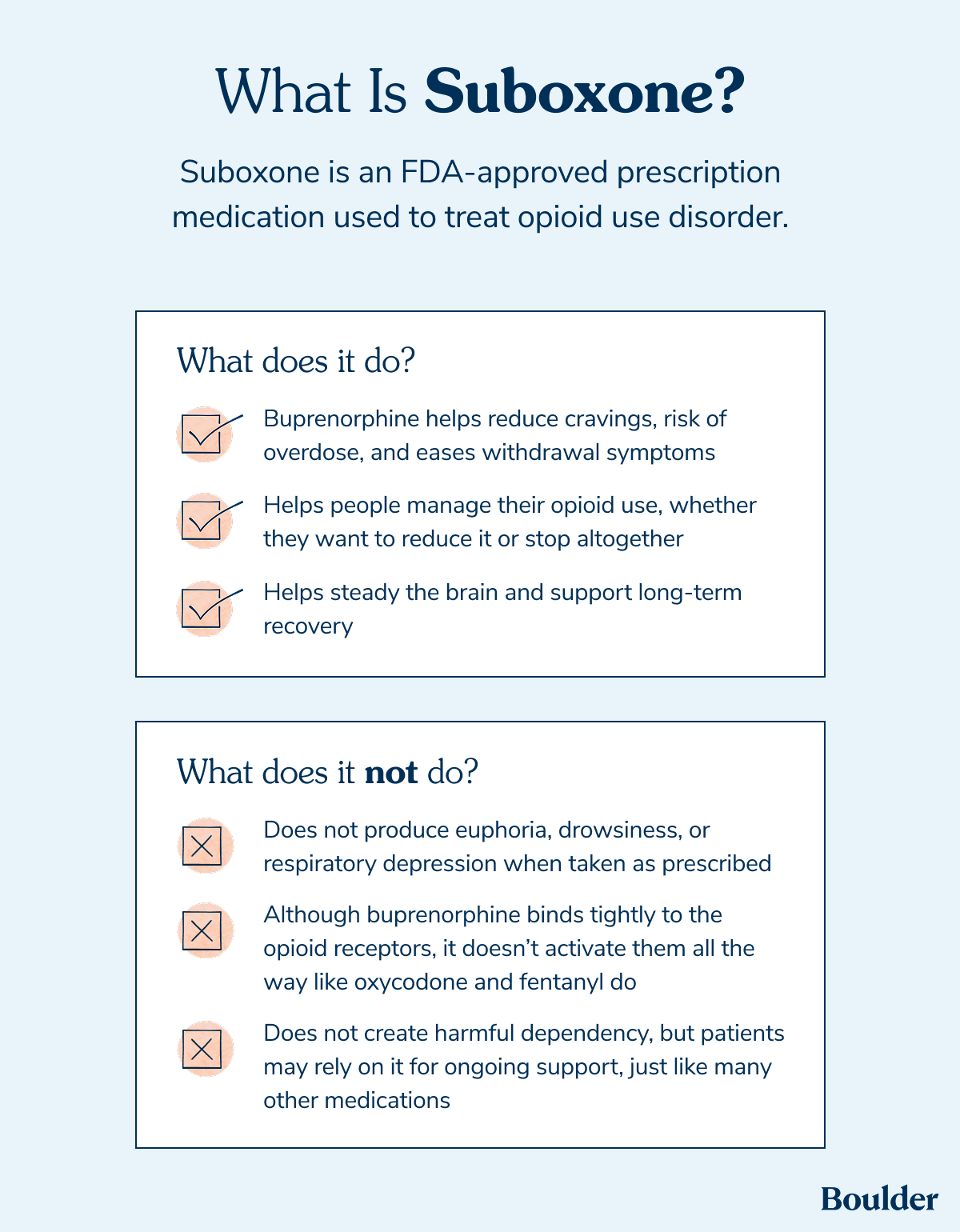
Suboxone is used to help people manage their opioid use, whether they want to reduce it or stop altogether. It is approved by the U.S. Food and Drug Administration (FDA) for this purpose. While Suboxone is not a one-time cure, it serves as a powerful partner in your recovery. By providing relief from withdrawal and calming cravings, it helps you stay safe and creates stability as you move forward in your journey.
“Buprenorphine is one of the most effective medications we have in all of medicine. Study after study shows it helps people with opioid use disorder live longer, healthier lives,” Dr. Appa says.
Because it works more gently on the brain than drugs like heroin, fentanyl, or prescription painkillers, it can help stop the cycle of feeling sick, using opioids, and then crashing again. For many people, this makes it easier to avoid overdose and get back to daily life, including focusing on work, relationships, and health.
Suboxone may not be recommended in some situations, including when:
Your Boulder Care provider will partner with you to determine if Suboxone is the best path forward, or if a different approach feels more like the right fit for your life. Beyond daily medication, we also offer long-acting options like Sublocade and Brixadi in most states, ensuring you have a choice in how you manage your recovery.
Suboxone works by changing how opioids affect the brain and body. Understanding how it works can help family members and other support people feel more confident about why it’s used.
It’s also helpful to know exactly what's in Suboxone. It contains two medicines that work together:
If Suboxone is taken improperly, it can cause unpleasant or potentially dangerous effects. These can include sudden withdrawal symptoms, breathing problems, or other serious side effects, especially if it is mixed with alcohol or sedatives like benzodiazepines.
When taken as prescribed, Suboxone is a safe and reliable tool that balances brain chemistry and provides the stability needed for lasting recovery.
"One thing I hear from patients is that buprenorphine helps the world feel clearer. Instead of feeling sedated, they feel a bit more alert and present. For some, that clarity is exactly what they need. For others, it takes getting used to," Dr. Appa explains.
Suboxone is taken by placing a film or tablet under the tongue (or sometimes inside the cheek), where it slowly dissolves. This allows the medication to absorb properly and work to reduce cravings and withdrawal symptoms throughout the day. Other forms of buprenorphine, such as Sublocade and Brixadi, are available as extended-release injections.
When Suboxone is working, people often notice several positive changes. Research shows that using Suboxone for opioid use disorder can reduce cravings, withdrawal, and the risk of overdose, particularly when treatment is used for a year or longer.
When people use Suboxone as a medication for opioid use disorder (MOUD), it makes overdoses and serious health problems less likely. Research has found that people taking buprenorphine or methadone had about a 76% lower risk of overdose at 3 months, and a 59% lower risk at 12 months compared to people who were not receiving MOUD.
Another study found that every 100 days of treatment with buprenorphine was linked to a 36% lower risk of opioid overdose compared to not receiving any medication.
People who stay in treatment longer tend to have better outcomes. Suboxone can help with that. In one study, each additional month of treatment was associated with about a 25% lower risk of using nonprescribed opioids. Evidence shows that people who take buprenorphine are more likely to stay in treatment compared to those who don’t receive medication.
People who continue taking buprenorphine for over a year are less likely to experience hospitalizations and emergency room visits compared to those who stop taking medication earlier.
Suboxone helps people use fewer opioids by lowering cravings and making withdrawal easier. This makes it much less likely that people will go back to using opioids.
In one study, people taking Suboxone were less likely to test positive for opioids. They also had more days in a row without using drugs and fewer cravings. This shows that taking Suboxone can help people use fewer opioids.
Everyone is different, but most people say these medicines help them feel much better. When you aren’t fighting cravings, it is easier to do the things you love, like:
A survey of treatment providers found that reduced cravings and illicit drug use were the most often cited benefits of buprenorphine and other opioid medications.
Suboxone can also help people who are dependent on kratom. Kratom is an herbal product—that comes from the leaves of the Mitragyna speciosa tree—that works on the same receptors as opioids, and people may feel sick when they try to stop taking it.
Some research has shown that buprenorphine and naloxone (the medications in Suboxone) can help people stop using kratom. This is an off-label use, but it shows that Suboxone can sometimes help people regain control when kratom use feels hard to manage.
There's a lot of mixed messaging around Suboxone and opioid treatment in general. A lot of that comes from outdated beliefs about recovery that don't always line up with real life. Before getting into the details of treatment, it helps to clear up a few common myths that often cause confusion.
Suboxone is also an opioid, so there’s a common misconception that taking it is just replacing one thing for another. But taking prescribed medication is not the same as uncontrolled opioid use.
"That idea comes from stigma, not science,” explains Patricia Pechter, MD, DABFM, a clinical quality improvement physician at Boulder Care. “Suboxone isn’t a substitute for getting high; it’s a treatment for a medical condition. Like insulin for diabetes or inhalers for asthma, it’s an FDA-approved medication that helps stabilize the brain and reduce cravings so people can rebuild their lives.”
Studies actually show that people who take Suboxone are more stable and less likely to experience an overdose, which is a primary goal of treatment.
While people often use the words addiction and dependence to describe drug use, they don’t mean the same thing.
While the body can become physically dependent on Suboxone–much like it does with medicine for blood pressure or diabetes–it’s important to remember that this is very different from the cycle of addiction. Instead of losing control, Suboxone actually helps you regain control. It provides the physical stability your body needs to function well, stay healthy, and live safely.
Some people believe that willpower or behavioral treatments should be enough to quit using drugs. While willpower is an important part of any journey, it’s often not enough on its own to overcome the physical changes opioids cause in the brain.
Opioid use disorder is a chronic brain condition, not a choice. Suboxone helps to heal some of those changes, providing a foundation that allows the behavioral treatments and your own determination to truly succeed.
Using medicine to help you get better is not ‘cheating’ and it does not make you weak. It is a smart, medical choice that works. Just like someone with asthma uses an inhaler to breathe, you are using a tool to stay healthy. This medicine helps you stick to your goals and keeps you safe.
There’s no “right” timeline for recovery. Some people stay on Suboxone for months, while others continue using it for years. Research has shown that longer use is linked to better safety outcomes. There is no set timeline for stopping medication. It’s a decision people make with their doctor based on what feels right for their situation.
“Suboxone helps people move toward health, stability, and recovery. Many stay on it for years and do very well. Others taper off when they’re ready if that’s their goal. Either way, it’s a tool that works,” Dr. Pechter says.
Suboxone can help anyone who uses opioids more than they’d like to or feels that they want to get out of a cycle of use that they can’t control. Early support can be helpful.
One study found that people who started buprenorphine-naloxone treatment within 30 days of their opioid use disorder diagnosis had much better results than people who started later. Early treatment was associated with a 42% lower risk for opioid overdose and a 51% lower risk of ER visits in the first year after diagnosis.
Research has found that people taking buprenorphine and naloxone were much less likely to show fentanyl in drug tests than those who were not in treatment. Even if you have used opioids, including fentanyl, for a long time or in large amounts, this medicine can still work for you. You may need to start the medication slowly, very quickly, or even need a higher dose of Suboxone.
Boulder offers same-day virtual care with no judgment, something that Dr. Pechter says is surprisingly rare in addiction treatment. The process is simple, and it takes place entirely on your phone. It means no sitting in waiting rooms or driving across town. You can talk to your doctor at home or wherever you feel safest.
“You download the app, complete onboarding, and meet with a clinician to create a plan that fits your goals. We consistently get feedback from patients that if they knew how straightforward it would be to get into Boulder Care, they would have tried it a long time ago,” Dr. Pechter says.
Here's what your journey might look like:
The first step is called "induction." It's the initial stage of treatment where someone transitions from taking opioids to taking Suboxone. This process helps get your body used to Suboxone in a way that minimizes withdrawal symptoms and sets you up for long-term success.
Treatment induction will be individualized for your needs. Some people follow a standard start schedule, while others opt to explore newer options like Boulder's QuickStart method, which makes the transition faster and more predictable.
You may feel unsettled and uncomfortable before Suboxone has time to fully kick in. Remember, Medical Assistants and clinicians are there to help, adjust dosing, and offer supportive meds if needed.
“We support people through the transition onto Suboxone, including prescribing medications to ease withdrawal and helping them control the pace of starting treatment,” Dr. Pechter explains. “That flexibility makes a big difference, especially for people who struggled with Suboxone in the past.”
The stabilization phase involves finding what works best for you. You'll work with your clinician to fine-tune your dose and schedule so that you can start to feel life returning to normal.
Once your body is responding well to Suboxone and the cravings are reduced, you enter the maintenance phase, where your medication helps support your daily routines.
Recovery isn't a one-and-done process. Each person’s experience is different. Some people take Suboxone for months, others for years. Staying connected with support, even as you gradually need less intensive care, can reduce risk and improve stability.
Recovery takes time. There will be good days, hard days, and everything in between, and Boulder is here to make sure you have the support you need.
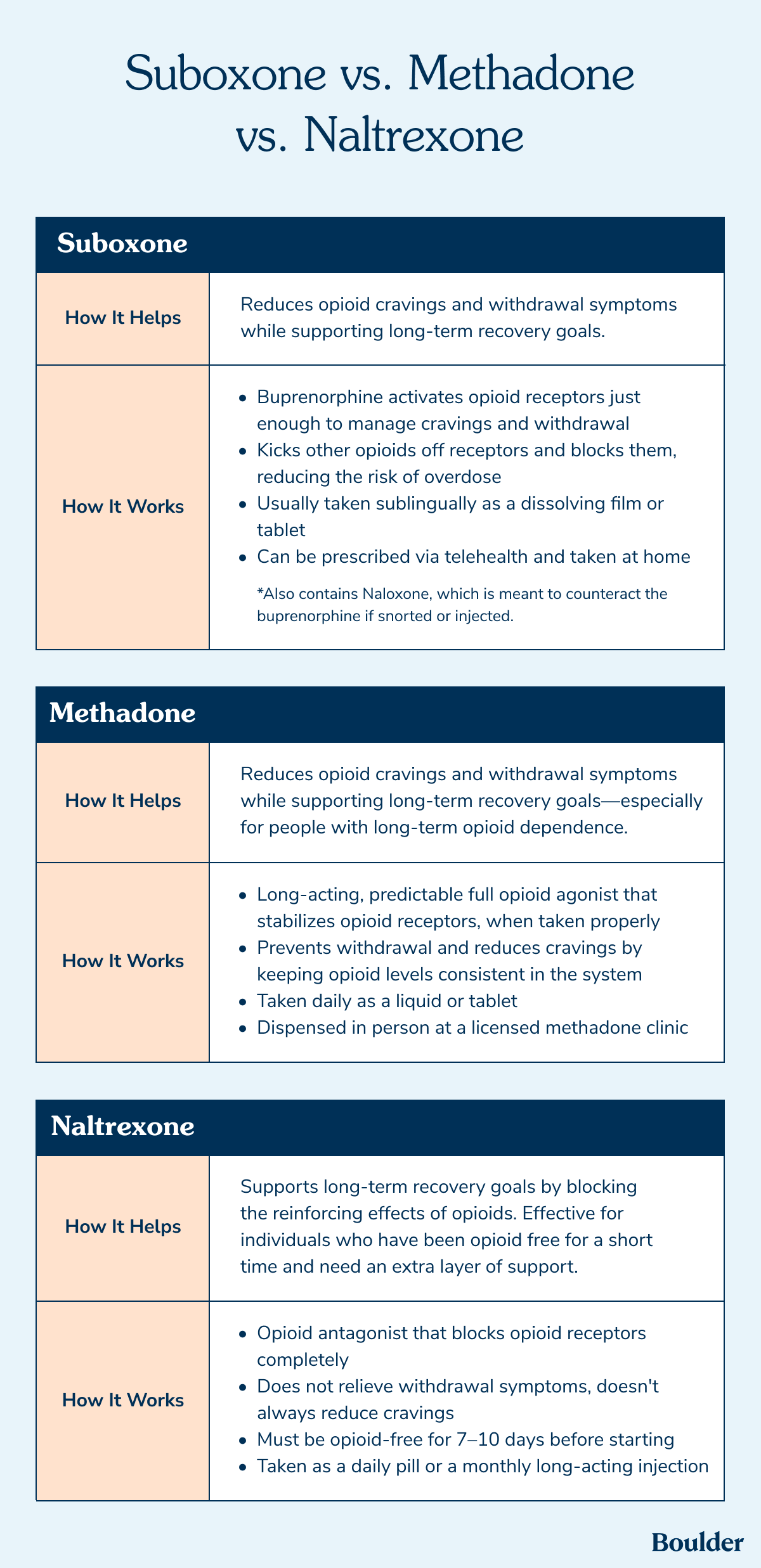
Three medications have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of opioid use disorder: buprenorphine, methadone, and naltrexone. All three have been shown to be effective and safe.
There isn’t one medication that’s right for everyone. “Each works differently, and the right choice depends on someone’s body, circumstances, and goals,” Dr. Pechter says.
We should have a solid understanding of Suboxone at this point, but for a quick recap:
Now let's take a closer look at the other two:
Methadone is a long-acting opioid that also reduces withdrawal and cravings. It can be helpful for people who have used opioids heavily or for a long time.
How it's used:
Methadone is often used if other medications haven't worked well or if a person would benefit from structured, daily support. “Methadone is effective, especially for people with severe opioid use disorder, but it’s tightly regulated,” Dr. Pechter explains. “Daily visits to a clinic, often for months, can make it hard to fit into real life, especially without reliable transportation. For some, the nearest methadone clinic would be hours away. “
Naltrexone blocks opioids so that they don't have an effect if they are used. It does not help ease withdrawal and may not reduce cravings for everyone.
How it's used:
Dr. Pechter notes that needing to be entirely off opioids for 7 to 10 days can be a major barrier. "There’s also a higher overdose risk after stopping due to reduced opioid tolerance," she says.
All three medications can be helpful tools. What works best isn’t the same for everyone, and it can change as your goals, needs, and access to care change.
Suboxone can help reduce cravings and lower overdose risk, making everyday life easier to manage for many people. Because it’s flexible, it works well with real-world challenges like pharmacy delays, stress, or changes in use. Staying connected to care can help with safety and long-term stability.
“Recovery isn’t one-size-fits-all. The goal isn’t to follow a script. We want to help you build a life that works for you. We’re here to support that, with evidence-based care, respect, and options that meet people where they are,” Dr. Pechter says.
If you're curious about whether Suboxone could be a good fit, Boulder is here to help. Call 888-422-6530 to speak with a care team member and learn more about getting started.
Yes, Suboxone is considered a narcotic because it contains buprenorphine, which affects the same receptors as other opioids. But it's different from drugs like heroin, or oxycodone. Buprenorphine doesn’t turn on these receptors all the way, so it's safer and doesn't give the same rush or intense euphoria. It's still a controlled medication. It can help treat illness, but it still has risks if it’s used the wrong way.
Just like other medicines, Subox can have side effects. Some people get things like headaches, nausea, trouble sleeping, or constipation. Starting too soon can cause withdrawal, so working with your provider closely to get the time right is important. It needs to be taken as prescribed, so stopping too quickly can be uncomfortable. These side effects are manageable for most people, so the pros usually outweigh the cons.
Yes, many insurance plans cover Suboxone, but coverage varies by plan and policy. Some plans may require prior authorization or have limits on the amount covered. Boulder accepts many different health insurance plans, including Medicaid and Medicare. Out-of-pocket payments are also accepted in select states. Check to see if we take your insurance or explore our self-pay options.
Opioid antagonists are medications that block the effects of opioids in the brain. They can prevent overdoses or reverse the effects of opioids. Some common examples include naloxone (the active ingredient in Narcan) and naltrexone.
There is no strict time limit for how long someone can stay on Suboxone. Some people use it for a few months, and others stay on it for a year or longer. Longer treatment can reduce the risk of overdose, hospitalizations, and opioid use.
While Suboxone contains naloxone, Subutex, Sublocade, and Brixadi only contain buprenorphine. Subutex was discontinued in the U.S., but buprenorphine is still widely used for opioid treatment as Suboxone, or in long-acting injections like Sublocade and Bixadi.